The journey of a blood clot from the leg to the lungs, known as a pulmonary embolism, can vary in speed depending on various factors such as clot size, individual physiology, and the presence of underlying medical conditions. Typically, a clot originating in the leg can take hours to days to travel to the lungs.
However, in certain circumstances, such as in the case of a large or particularly mobile clot, this journey can occur more rapidly, potentially leading to severe complications. Understanding the dynamics of clot migration is crucial for timely diagnosis and intervention to prevent life-threatening consequences.
What is a blood clot?
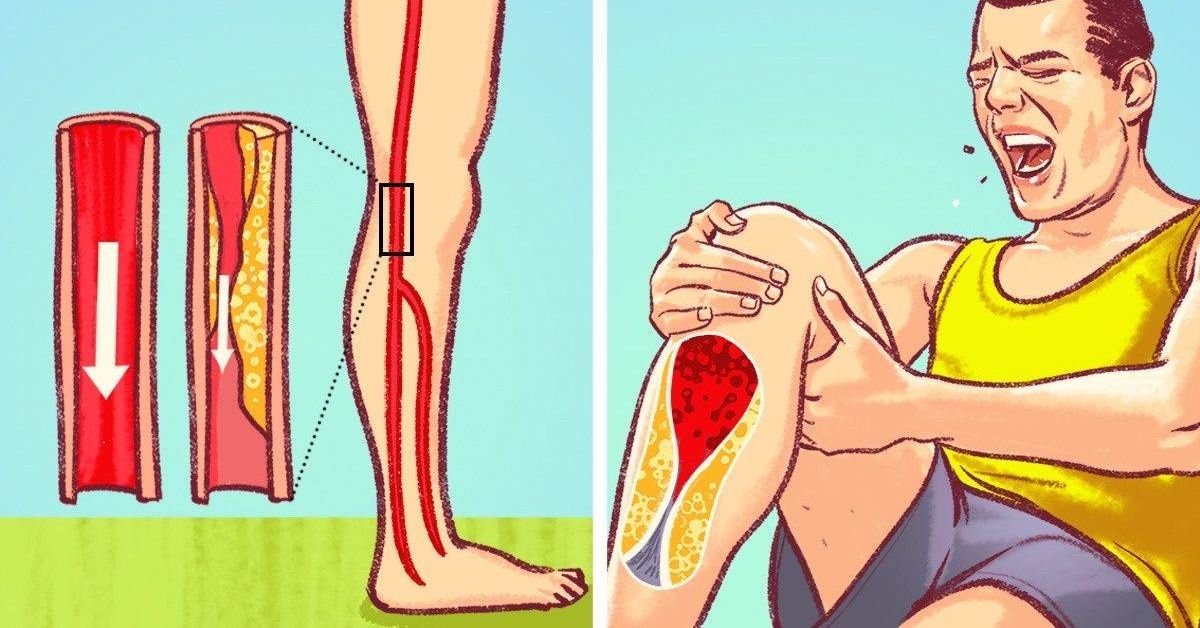
A blood clot, also known as a thrombus, is a semi-solid mass of blood that forms when the body’s clotting mechanism is activated. Clotting is a normal and necessary process that helps to prevent excessive bleeding when a blood vessel is injured. However, sometimes clots can form inside blood vessels without an apparent injury, which can be dangerous.
When does a blood clot become dangerous?
A blood clot becomes dangerous when it blocks the flow of blood through a blood vessel. This can happen in various parts of the body, including the legs, arms, lungs, heart, and brain. When a clot blocks a blood vessel, it can deprive the surrounding tissues of oxygen and nutrients, potentially leading to tissue damage or organ failure.
How fast can a PE blood clot travel?
A pulmonary embolism (PE) is a potentially life-threatening condition that occurs when a blood clot travels from another part of the body, such as the leg or arm, to the lungs and blocks one or more blood vessels. The speed at which a blood clot can travel from the leg to the lungs can vary, but it is generally a relatively rapid process.
According to medical experts, a blood clot can travel from the leg to the lungs in a matter of seconds or minutes, depending on various factors. The speed of travel is influenced by several factors, including the size of the clot, the location of the clot within the venous system, and the individual’s cardiovascular health and blood flow.
Larger clots may travel more slowly than smaller ones, as they can become lodged more easily in the narrower blood vessels. However, even small clots can cause significant blockages in the lung’s blood vessels, leading to a pulmonary embolism.
Blood Clots and Travel: What You Should Know
Long periods of immobility, such as during long-haul flights or extended car journeys, can increase the risk of developing blood clots, particularly in the legs. This is because the lack of movement can cause blood to pool in the lower extremities, increasing the chances of clot formation.
If you are planning to travel, it is essential to take precautions to reduce your risk of developing blood clots. Here are some tips:
- Stay hydrated by drinking plenty of water during your journey.
- Wear loose-fitting, comfortable clothing that does not restrict blood flow.
- Engage in periodic leg exercises and stretches to promote circulation.
- Consider wearing compression stockings, which can help improve blood flow in the legs.
- If you have a history of blood clots or other risk factors, consult with your healthcare provider before traveling.
Read This Blog: BlueFire Wilderness Therapy Reviews: A Comprehensive Guide
Understand What Can Increase Your Risk for Blood Clots
While anyone can develop a blood clot, certain factors can increase an individual’s risk. Understanding these risk factors can help you take proactive measures to reduce your chances of developing a clot. Some of the most common risk factors include:
- Age: The risk of blood clots increases as you get older, particularly after the age of 60.
- Obesity: Being overweight or obese can put additional strain on your circulatory system and increase the likelihood of clot formation.
- Smoking: Smoking can damage blood vessel walls and increase the risk of clotting.
- Pregnancy and hormonal birth control: Hormonal changes during pregnancy and the use of certain birth control methods can increase the risk of clot formation.
- Cancer and cancer treatments: Some types of cancer and certain cancer treatments, such as chemotherapy, can increase the risk of blood clots.
- Immobility: Prolonged periods of inactivity, such as after surgery or during long-distance travel, can contribute to the development of clots.
- Family history: If you have a close relative who has experienced blood clots, you may be at a higher risk.
It is essential to discuss your individual risk factors with your healthcare provider to develop an appropriate prevention and management plan.
Do all blood clots travel and become dangerous?
Not all blood clots travel or become dangerous. In fact, many clots remain localized and do not pose a significant threat to health. However, it is important to be aware of the potential risks and seek medical attention if you experience symptoms that may indicate the presence of a blood clot.

Clots that form in the deep veins of the legs or arms, known as deep vein thrombosis (DVT), are particularly concerning because they have the potential to break off and travel to the lungs, causing a pulmonary embolism (PE). PEs can be life-threatening if not treated promptly.
It is also possible for blood clots to form in other parts of the body, such as the heart or brain, which can lead to serious complications like heart attacks or strokes.
How to prevent blood clots in the first place!
While it is important to be aware of the potential risks and symptoms of blood clots, it is equally crucial to take proactive steps to prevent them from occurring in the first place. Here are some effective strategies for blood clot prevention:
- Stay active: Regular physical activity helps promote healthy blood flow and reduces the risk of clot formation. Aim for at least 30 minutes of moderate exercise most days of the week.
- Maintain a healthy weight: Being overweight or obese increases the risk of blood clots. Adopt a balanced diet and exercise regimen to maintain a healthy body weight.
- Quit smoking: Smoking can damage blood vessel walls and increase the risk of clotting. If you smoke, consider quitting with the help of a healthcare professional or smoking cessation program.
- Stay hydrated: Dehydration can thicken the blood and increase the risk of clot formation. Drink plenty of water and fluids throughout the day.
- Manage underlying conditions: If you have conditions that increase the risk of blood clots, such as diabetes, heart disease, or cancer, work closely with your healthcare provider to manage these conditions effectively.
- Take medication as prescribed: If you have been prescribed medications to prevent blood clots, such as anticoagulants (blood thinners), it is essential to take them as directed by your healthcare provider.
- Compression stockings: For individuals at high risk for blood clots, wearing compression stockings can help improve blood flow in the legs and reduce the risk of clot formation.
By implementing these preventive measures, you can significantly reduce your risk of developing dangerous blood clots and maintain good cardiovascular health.
Also Read This Blog: How To Become A Travel Agent?
How much do you know about blood clots?
Blood clots can be a serious and potentially life-threatening condition, but many people are unaware of the risks, symptoms, and prevention strategies. Take this short quiz to test your knowledge about blood clots:
- True or False: Blood clots only occur in older adults.
- Which of the following is a risk factor for blood clots? a. Smoking b. Obesity c. Prolonged immobility d. All of the above
- Symptoms of a blood clot in the leg may include: a. Swelling b. Pain or tenderness c. Warmth or redness in the affected area d. All of the above
- If a blood clot travels to the lungs, it is called: a. Deep vein thrombosis (DVT) b. Pulmonary embolism (PE) c. Heart attack d. Stroke
- True or False: Drinking plenty of water can help prevent blood clots.
Are you concerned that you have a blood clot in the Leg? We can help!
If you are experiencing symptoms that may indicate the presence of a blood clot in your leg, such as swelling, pain, warmth, or redness, it is crucial to seek medical attention promptly. Blood clots in the legs, known as deep vein thrombosis (DVT), can be a serious condition that requires prompt treatment to prevent potentially life-threatening complications.
At our healthcare facility, we have a team of experienced healthcare professionals who are trained to evaluate and manage cases of suspected DVT. Our diagnostic procedures may include:
- Physical examination: Our healthcare providers will perform a thorough physical examination, checking for signs of swelling, tenderness, and discoloration in the affected area.
- Ultrasound imaging: An ultrasound scan can effectively detect the presence of blood clots in the veins of the leg, providing valuable diagnostic information.
- Blood tests: Certain blood tests may be
If a blood clot is detected, our healthcare team will work promptly to initiate appropriate treatment. This may include:
- Anticoagulant medication: Blood-thinning medications, such as heparin or warfarin, are commonly prescribed to prevent further clot formation and reduce the risk of complications.
- Compression stockings: Wearing compression stockings can help improve blood flow and prevent the clot from growing larger.
- Elevation and rest: Keeping the affected leg elevated and resting can alleviate symptoms and promote healing.
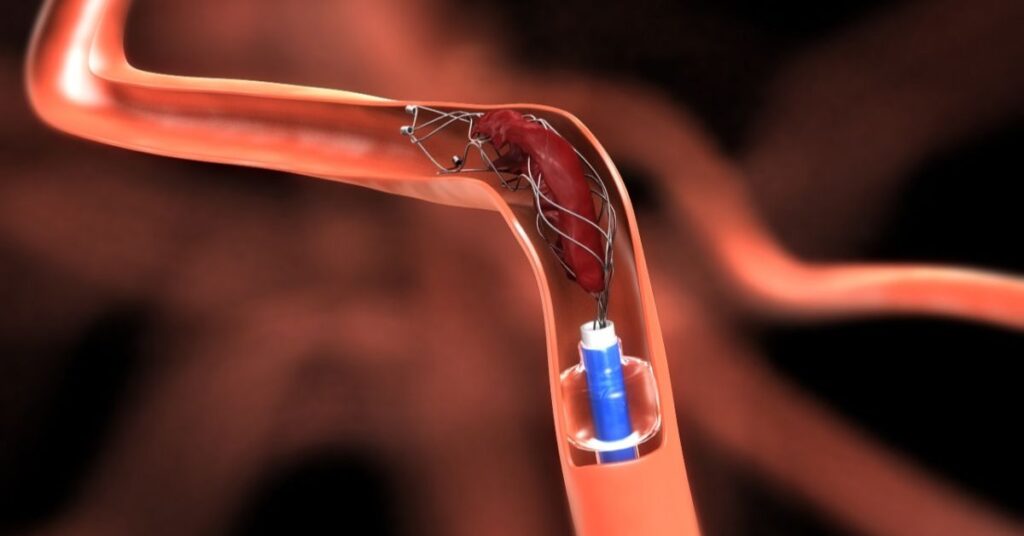
In some cases, more advanced treatments may be necessary, such as:
- Thrombolytic therapy: This involves administering clot-busting medications to dissolve the blood clot.
- Vascular surgery: In severe cases, surgical intervention may be required to remove or bypass the clot.
Early diagnosis and treatment are crucial for managing DVT effectively and preventing potential complications, such as pulmonary embolism (PE), which occurs when a clot travels to the lungs and can be life-threatening.
At our facility, we prioritize patient safety and well-being, and our team will work closely with you to develop a comprehensive treatment plan tailored to your specific needs and medical history.
Frequently asked questions
Can you physically see a blood clot?
In some cases, particularly with clots in superficial veins, it may be possible to see or feel a blood clot. However, for clots that form in deeper veins, such as those associated with deep vein thrombosis (DVT), physical signs may not be apparent. Medical imaging techniques, such as ultrasound or CT scans, are often necessary to detect and confirm the presence of a blood clot in these cases.
Can a blood clot go away on its own?
In some instances, smaller blood clots may dissolve on their own, especially if they are located in superficial veins. However, larger clots or those in deeper veins are less likely to resolve without medical intervention. It is crucial not to assume that a blood clot will go away on its own, as untreated clots can lead to serious complications, such as pulmonary embolism or tissue damage.
What are the first signs of a blood clot in the leg?
The most common early signs of a blood clot in the leg (deep vein thrombosis or DVT) include:
- Swelling, warmth, and tenderness in the affected leg
- Pain or discomfort, especially when walking or standing
- Redness or discoloration of the skin on the affected leg
It’s important to note that these symptoms may not always be present or may be subtle in some cases. If you experience any concerning symptoms, it is essential to seek medical attention promptly for proper evaluation and diagnosis.
How fast does a blood clot travel from the legs to the lungs?
The speed at which a blood clot travels from the legs to the lungs can vary significantly depending on various factors, such as the size of the clot, the individual’s cardiovascular health, and the presence of any underlying medical conditions.
In general, larger clots may travel more slowly than smaller ones, as they can become lodged more easily in narrower blood vessels. However, even small clots can cause significant blockages in the lung’s blood vessels, leading to a potentially life-threatening pulmonary embolism (PE).
According to medical experts, a blood clot can travel from the leg to the lungs in a matter of seconds or minutes in some cases, although the exact time can be difficult to predict. Prompt medical attention is crucial if you suspect the presence of a blood clot, as timely treatment can help prevent complications and potentially save lives.
How to check for a blood clot in your leg?
If you suspect you may have a blood clot in your leg, it is essential to seek medical attention promptly. A healthcare professional can perform various tests and examinations to check for the presence of a clot, including:
- Physical examination: Your healthcare provider will examine the affected leg for signs of swelling, warmth, tenderness, and discoloration, which can indicate the presence of a clot.
- Doppler ultrasound: This non-invasive imaging technique uses sound waves to visualize the veins in your leg and detect any blockages or clots.
- D-dimer blood test: This blood test measures the levels of a substance called D-dimer, which is produced when a clot breaks down. Elevated levels of D-dimer can indicate the presence of a clot.
- Venography: In this procedure, a contrast dye is injected into the veins of your leg, and X-ray images are taken to visualize the flow of blood and identify any blockages caused by clots.
It’s important not to attempt to self-diagnose or ignore persistent symptoms, as prompt medical evaluation and treatment are crucial for managing blood clots effectively and preventing potential complications.
What is the treatment for a blood clot in the leg?
The treatment for a blood clot in the leg, known as deep vein thrombosis (DVT), typically involves a combination of medications and lifestyle modifications. The primary goals of treatment are to prevent the clot from growing larger, reduce the risk of complications (such as pulmonary embolism), and prevent the formation of new clots.
Here are some common treatment options for DVT:
- Anticoagulant medications (blood thinners): These medications, such as heparin, warfarin, or direct oral anticoagulants (DOACs), are the mainstay of treatment for DVT. They work by preventing further clot formation and allowing the body’s natural mechanisms to gradually break down the existing clot.
- Compression stockings: Wearing compression stockings can help improve blood flow in the affected leg and prevent the clot from growing larger.
- Elevation and leg exercises: Keeping the affected leg elevated and performing gentle leg exercises can also help improve blood circulation and prevent complications.
- Thrombolytic therapy: In some cases, clot-busting medications (thrombolytics) may be administered to dissolve the clot more quickly, especially in severe or life-threatening situations.
- Vascular surgery: In rare cases, surgical intervention may be required to remove or bypass a large or persistent clot.
Treatment duration and specific medications used may vary depending on the individual’s risk factors, the severity of the clot, and the presence of any underlying medical conditions. It’s crucial to follow your healthcare provider’s instructions carefully and attend all follow-up appointments to monitor your progress and adjust the treatment plan as needed.
Conclusion
Understanding the risks, symptoms, and potential complications of blood clots is essential for maintaining good cardiovascular health. While blood clots can be potentially life-threatening, there are effective prevention strategies and treatments available.
By staying active, maintaining a healthy weight, managing underlying medical conditions, and being aware of the warning signs, you can significantly reduce your risk of developing dangerous blood clots. If you experience symptoms that may indicate the presence of a clot, it is crucial to seek prompt medical attention, as early diagnosis and treatment can greatly improve outcomes.
Brook, an intrepid explorer and seasoned hiker, has traversed rugged terrains worldwide. Through “hikingplayer,” He shares her adventures, insider tips, and passion for embracing nature’s wonders one trail at a time.